A structured dietary regimen combining plant-based eating principles with the specific nutritional needs of individuals managing diabetes, often accessed as a downloadable document in Portable Document Format (PDF), facilitates adherence to a controlled eating pattern. Such resources typically outline meal ideas, portion sizes, and nutritional information to aid in blood glucose regulation. An example would be a document detailing a seven-day eating schedule featuring recipes for breakfast, lunch, dinner, and snacks, all adhering to both vegan and diabetic guidelines.
The significance of such a dietary approach lies in its potential to improve glycemic control, reduce cardiovascular risk factors, and promote weight management in individuals with diabetes. Historically, managing diabetes often relied heavily on animal-based products. However, research suggests that well-planned plant-based diets, adhering to diabetic guidelines, can be equally effective, and in some cases, may offer additional advantages such as increased fiber intake and reduced saturated fat consumption. The accessibility afforded by the described downloadable format allows wider dissemination of information and greater individual control over meal planning.
The subsequent discussion will delve into the key considerations for developing and implementing a successful diet, exploring the types of foods to include and avoid, the importance of macronutrient balance, and strategies for managing blood glucose levels. Furthermore, the article will address common challenges encountered when following this specific dietary pattern and provide practical solutions to overcome them, all in the context of effectively managing diabetes.
Practical Guidance for Plant-Based Diabetes Management
The successful application of plant-based dietary principles for individuals with diabetes necessitates meticulous planning and adherence to established nutritional guidelines. The following points offer practical guidance for navigating this specific dietary approach.
Tip 1: Prioritize Whole, Unprocessed Foods: Emphasis should be placed on consuming whole grains, legumes, vegetables, and fruits in their least processed forms. For instance, choosing brown rice over white rice or whole fruits over fruit juice maximizes fiber intake and minimizes rapid blood glucose spikes.
Tip 2: Monitor Carbohydrate Intake: Consistent monitoring of carbohydrate consumption is critical for blood glucose control. Understanding the glycemic index and glycemic load of various foods can inform portion sizes and meal planning strategies. For example, combining high-carbohydrate foods with healthy fats and protein can slow down glucose absorption.
Tip 3: Ensure Adequate Protein Intake: Plant-based protein sources such as lentils, beans, tofu, and tempeh are essential for satiety and muscle maintenance. A balanced meal should include a sufficient serving of protein. Consider incorporating protein-rich foods into each meal, like adding tofu to a vegetable stir-fry.
Tip 4: Incorporate Healthy Fats: Unsaturated fats from sources such as avocados, nuts, seeds, and olive oil play a vital role in overall health and can improve insulin sensitivity. However, moderation is key due to their caloric density. A small handful of nuts or a drizzle of olive oil can be a beneficial addition to a meal.
Tip 5: Manage Portion Sizes: Even with healthful food choices, excessive portions can lead to elevated blood glucose levels. Utilize measuring tools to accurately determine appropriate serving sizes. Portion control containers or scales can be helpful in maintaining consistent meal sizes.
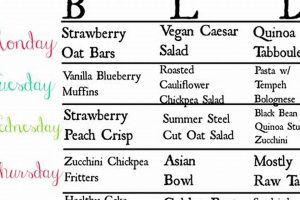
Tip 6: Plan Meals in Advance: Pre-planning meals helps prevent impulsive, less healthful food choices. Creating a weekly meal plan and preparing components in advance ensures that nutritious, diabetes-friendly options are readily available. Designating a specific time for meal preparation can facilitate this process.
Tip 7: Stay Hydrated: Adequate water intake is crucial for overall health and can aid in blood glucose regulation. Consuming water throughout the day, especially before and during meals, supports optimal metabolic function. A general recommendation is to drink at least eight glasses of water daily.
Following these recommendations facilitates the effective integration of plant-based eating patterns into diabetes management, offering the potential for improved glycemic control and overall well-being.
The subsequent section will provide further insights into potential challenges and strategies for overcoming them in the context of following a plant-based approach to diabetes management.
1. Accessibility
Accessibility, in the context of a plant-based eating guide for diabetes management, encompasses the ease with which individuals can obtain, understand, and implement the plan. A guide, regardless of its nutritional soundness, remains ineffective if individuals face barriers to its utilization. These barriers can manifest as limitations in access to the document itself, unclear or overly technical language, a lack of readily available ingredients, or prohibitive costs. For example, if the guide exists solely as a physical document unavailable online, individuals in remote areas or those with mobility issues are effectively excluded.
The Portable Document Format (PDF) is often employed due to its platform independence and ability to preserve formatting across different devices. However, even in this format, accessibility considerations remain crucial. Screen reader compatibility, the use of alt text for images, and ensuring sufficient color contrast are necessary for individuals with visual impairments. Furthermore, the language used must be clear, concise, and devoid of jargon. Complex medical terminology should be explained, and recipe instructions must be easy to follow. The recipes themselves should utilize ingredients that are readily available in most supermarkets and consider cost constraints, offering affordable alternatives where possible. For instance, suggesting locally sourced, seasonal produce can reduce both the cost and environmental impact of the diet.
Ultimately, accessibility is not merely about providing information; it is about empowering individuals to make informed choices and successfully manage their diabetes through dietary modifications. Challenges related to accessibility can be mitigated through careful planning, inclusive design, and a focus on the practical needs of the target audience. Without a commitment to accessibility, the potential benefits of a plant-based eating guide for diabetes management are significantly diminished, hindering its effectiveness in improving health outcomes.
2. Nutritional Adequacy
The nutritional adequacy of a plant-based eating guide for diabetes is paramount to its efficacy and safety. A document lacking in crucial nutrients, despite adhering to vegan principles and diabetic guidelines, can lead to deficiencies and adverse health outcomes. Therefore, the creation and assessment of such guides must prioritize the provision of all essential macro- and micronutrients in appropriate quantities. The core concept revolves around ensuring the plan provides sufficient protein, healthy fats, complex carbohydrates, fiber, vitamins (such as B12 and D), and minerals (including iron, calcium, and zinc), all while maintaining appropriate blood glucose control.
The construction of an adequate vegan diabetic meal plan addresses numerous factors. Firstly, it necessitates a thorough understanding of nutrient bioavailability in plant-based foods. For example, iron from plant sources (non-heme iron) is less readily absorbed than heme iron from animal products. Strategies to enhance iron absorption, such as consuming iron-rich foods alongside vitamin C-rich foods, must be integrated into the meal plan. Likewise, vitamin B12, typically found in animal products, needs to be supplemented or obtained from fortified foods to prevent deficiency. Regarding protein, the guide should advocate for combining diverse plant-based protein sources, such as legumes, grains, nuts, and seeds, to ensure a complete amino acid profile. A meal plan that does not adequately address these considerations could lead to significant nutritional gaps, counteracting the potential benefits of the dietary approach. Deficiencies could then lead to fatigue, weakened immunity, and potentially severe complications.
In conclusion, the provision of complete and balanced nutrition within a downloadable plant-based guide for diabetic individuals is critical. Careful planning, attention to detail, and awareness of nutrient interactions are essential to prevent deficiencies and ensure the plan’s effectiveness and safety. Meal plans lacking a sound nutritional foundation may not meet the needs of those relying on them, and may potentially lead to serious health complications. Regular consultation with a registered dietitian or certified diabetes educator is encouraged to personalize and monitor the nutritional adequacy of the selected meal plan, to prevent deficiencies and adjust based on individual requirements.
3. Glycemic Control
Glycemic control, the maintenance of stable blood glucose levels within a target range, is a central objective in diabetes management. A plant-based eating plan, often accessed in PDF format, represents a potential tool for achieving this goal. The inherent characteristics of many plant-based foods, such as high fiber content and low glycemic index, can positively influence postprandial glucose responses. Fiber slows down the absorption of glucose from the digestive tract, preventing rapid spikes in blood sugar. The selection of low-glycemic index foods, like legumes and non-starchy vegetables, further contributes to stable glucose levels. A downloadable meal plan offering specific portion sizes and meal timings allows individuals to consistently apply these principles. Failure to incorporate strategies for optimized glycemic control within such a plan renders it inadequate for its intended purpose. For example, a meal plan featuring solely high-glycemic fruits or refined grains, even within a plant-based framework, would likely result in poor blood sugar regulation.
The practical application of a plant-based eating regimen for glycemic control demands careful consideration of macronutrient ratios and food combinations. A well-designed guide balances carbohydrate intake with sufficient protein and healthy fats, further stabilizing blood glucose. Furthermore, understanding the concept of glycemic load, which considers both the glycemic index of a food and its carbohydrate content per serving, is crucial. Individuals using such documents should be educated on how to adjust their food choices and portion sizes based on their individual blood glucose responses. Real-world examples of improved glycemic control through plant-based eating can be observed in clinical trials, where participants adhering to such diets often exhibit reduced HbA1c levels, a marker of long-term blood glucose control. Such improvements contribute to reduced risks of diabetic complications, like cardiovascular disease and neuropathy.
In summary, the association between glycemic control and a downloadable document detailing a plant-based eating approach for diabetes is integral. Such documents must prioritize the inclusion of low-glycemic index foods, adequate fiber, balanced macronutrients, and practical strategies for blood glucose monitoring and adjustment. Ignoring the principles of glycemic control within this context undermines the plans ability to effectively manage diabetes and prevent associated complications. The challenges lie in the need for personalized guidance, ongoing education, and consistent adherence to the principles outlined in the plan, all contributing to the successful management of blood glucose levels within the desired range.
4. Recipe Variety
Recipe variety is a critical component of a usable and sustainable plant-based eating guide for individuals with diabetes, often accessed as a PDF. The diversity of meals presented within these guides directly impacts adherence, nutritional intake, and overall satisfaction with the dietary approach.
- Nutrient Diversity
A broad range of recipes ensures adequate intake of all essential nutrients. Restricting the diet to a limited set of meals can increase the risk of nutrient deficiencies, even within a carefully planned dietary approach. For example, focusing only on leafy green salads as the sole source of vegetables may result in low intake of certain vitamins and minerals found in other types of vegetables. A diverse guide integrates recipes utilizing a wide array of ingredients to ensure nutritional completeness.
- Palatability and Satisfaction
The appeal of recipes directly affects the likelihood of adherence to the diet. A monotonous meal plan can lead to boredom and ultimately, abandonment of the dietary approach. Examples might include incorporating a variety of flavors and textures, ranging from savory to sweet, and from crunchy to creamy. The inclusion of global cuisines and innovative cooking techniques can enhance enjoyment and make the diet more sustainable. The plan must not only be nutritionally sound, but also encourage users to adhere to it long-term.
- Adaptability to Preferences and Allergies
A versatile guide acknowledges the diversity of individual food preferences and potential allergies or intolerances. Offering variations of recipes to accommodate different tastes and dietary needs ensures that the plan can be tailored to suit individual circumstances. For example, a recipe might offer substitutions for specific vegetables or grains based on availability, seasonality, or individual preferences. This adaptability increases the accessibility and usability of the plan, making it suitable for a wider range of individuals.
- Cultural Relevance
Adapting to cultural and local foodways can greatly improve adherence. Meal plans that consider the dietary habits of specific communities, and offer substitutions and variations that take these elements into consideration, make the plan more approachable. A one-size-fits-all meal plan for all communities can lead to quick abandonment and is not culturally relevant.
The integration of recipe variety within a downloadable guide significantly contributes to the long-term success of plant-based dietary management for diabetes. By addressing nutrient diversity, palatability, adaptability, and cultural sensitivity, the plan becomes a more sustainable and effective tool for individuals seeking to manage their condition through dietary modifications. These elements ensure that the eating guide is used for the long term.
5. Portion Guidance
Accurate portion guidance within a plant-based dietary regimen for diabetic individuals, often provided as a Portable Document Format (PDF), is critical for effective glycemic control and weight management. The causal relationship between portion size and blood glucose levels is direct: larger portions of carbohydrate-containing foods lead to higher postprandial glucose excursions. Therefore, the absence of explicit portion recommendations within such a guide diminishes its utility in managing diabetes. For example, a meal plan featuring a recipe for lentil soup, but failing to specify serving size, offers limited practical benefit to an individual seeking to regulate their blood sugar levels. It’s critical to note that even healthy foods, consumed in excessive amounts, can adversely affect blood glucose.
The incorporation of detailed serving sizes and suggested meal compositions transforms a general dietary framework into a concrete, actionable plan. A guide might specify that a serving of brown rice should be half a cup cooked, or that a portion of tofu stir-fry should contain four ounces of tofu. Furthermore, visual aids, such as photographs illustrating appropriate portion sizes, can enhance understanding and compliance. Such measures provide a framework by which individuals are able to more effectively self-manage their diets. Also, the guide provides the user with actionable steps that they can follow when portioning their food.
In conclusion, portion guidance serves as an indispensable element within a plant-based strategy for diabetes management. Its inclusion within a downloadable PDF enhances the guide’s effectiveness by providing concrete, actionable information for blood glucose and weight management. Without this element, the meal plan would be rendered less effective and less helpful for its intended users.
6. Long-Term Adherence
Long-term adherence represents a critical determinant of the success of any dietary intervention, particularly a plant-based eating plan for individuals managing diabetes. A downloadable document detailing such a plan, regardless of its nutritional soundness or initial effectiveness, yields limited benefit if individuals cannot consistently follow it over extended periods. The correlation between adherence and positive health outcomes is well-established; sustained adherence to a well-designed plan typically results in improved glycemic control, reduced cardiovascular risk, and enhanced overall well-being. Conversely, sporadic or short-term adherence often fails to produce significant or lasting improvements in health status. For instance, individuals who initially experience positive results from a carefully structured plant-based diet but subsequently revert to previous eating habits may observe a return of elevated blood glucose levels and an increase in associated health risks.
Factors influencing long-term adherence to a plant-based eating plan for diabetes are multifaceted and encompass individual preferences, social support, cultural considerations, and the perceived practicality of the plan itself. A resource that fails to address these factors is unlikely to promote sustained behavioral change. For example, a downloadable PDF featuring complex recipes requiring specialized ingredients and extensive preparation time may prove impractical for individuals with demanding schedules or limited culinary skills, leading to eventual abandonment of the plan. Similarly, a plan that clashes with cultural food preferences or lacks the support of family members may encounter significant resistance. The key lies in creating a flexible, adaptable, and sustainable approach that integrates seamlessly into an individual’s lifestyle. For some, weekly meetings with a nutritionist and family support is necessary to stay on the path.
In conclusion, long-term adherence constitutes an essential element in the effective implementation of a plant-based dietary strategy for diabetes management. A downloadable guide designed to promote such adherence must consider individual needs, practical limitations, and cultural factors. By prioritizing flexibility, personalization, and ongoing support, such resources can significantly enhance the likelihood of sustained behavioral change and the realization of long-term health benefits. A well crafted guide will empower the individual for successful blood glucose control for long-term health.
Frequently Asked Questions
The following questions address common concerns and misconceptions surrounding plant-based eating plans, particularly as they pertain to individuals managing diabetes. The answers provide factual information and evidence-based recommendations to assist in informed decision-making.
Question 1: Are plant-based diets safe for individuals with diabetes?
When implemented thoughtfully and under the guidance of qualified healthcare professionals, plant-based diets are considered safe for individuals with diabetes. These diets often improve glycemic control, reduce cardiovascular risk factors, and promote weight loss. A well-structured plan ensures adequate nutrient intake and addresses specific needs for individuals with diabetes. Professional guidance is still needed, however, to ensure the individual receives the right plan for them.
Question 2: Will a plant-based diet provide sufficient protein for someone with diabetes?
Plant-based diets can supply adequate protein when properly planned. Sources include legumes (beans, lentils, peas), tofu, tempeh, nuts, seeds, and whole grains. Combining these sources ensures the intake of all essential amino acids. The protein requirements are achieved with careful dietary considerations.
Question 3: How does a plant-based diet impact blood glucose levels in individuals with diabetes?
Plant-based diets, characterized by high fiber content and low glycemic index foods, can improve blood glucose control. Fiber slows glucose absorption, preventing rapid spikes in blood sugar. The selection of low-glycemic index foods helps maintain stable glucose levels. Overall, there is improved control for people with well planned diets.
Question 4: Is vitamin B12 supplementation necessary on a plant-based diet for diabetes management?
Vitamin B12 is not reliably found in plant-based foods. Supplementation or consumption of fortified foods is generally necessary to prevent deficiency, especially for long-term adherence to a plant-based diet. Deficiency can lead to neurological problems and anemia; therefore, supplementation must occur.
Question 5: Can a plant-based diet effectively manage type 1 diabetes?
With diligent carbohydrate counting, insulin adjustments, and close monitoring of blood glucose levels, plant-based diets can be safely and effectively managed in type 1 diabetes. Close collaboration with an endocrinologist and registered dietitian is essential. There are a series of actions that need to occur for this to be successful.
Question 6: What are the potential risks of a poorly planned plant-based diet for individuals with diabetes?
Poorly planned plant-based diets can lead to nutrient deficiencies (e.g., vitamin B12, iron, calcium), inadequate protein intake, and poor glycemic control. Consulting with a healthcare professional is crucial to ensure nutritional adequacy and prevent adverse outcomes. With professional guidance, problems can be avoided.
A plant-based diet can be a safe and effective approach to diabetes management with proper planning and healthcare professional guidance. Attention to nutrient needs and glycemic control is essential.
In the subsequent discussion, real-world examples, practical tips, and further guidance will be provided for adopting and sustaining a plant-based eating plan for diabetes management.
Conclusion
This article has explored the multifaceted implications of a “vegan diabetic meal plan pdf” as a tool for managing diabetes. The documented dietary approach offers potential benefits, including improved glycemic control and enhanced nutritional intake. However, the success of such plans hinges on several crucial factors: accessibility, nutritional adequacy, glycemic control, recipe variety, portion guidance, and long-term adherence. Failure to adequately address these considerations can diminish the effectiveness and safety of the dietary intervention.
The implementation of a “vegan diabetic meal plan pdf” warrants careful planning, individualization, and ongoing monitoring by qualified healthcare professionals. Such resources can provide a framework for dietary change, but should not be considered a substitute for personalized medical advice. Individuals considering this dietary approach are urged to seek guidance from registered dietitians or certified diabetes educators to ensure optimal health outcomes. The potential for successful diabetes management exists with these resources but necessitates a commitment to informed decision-making and professional oversight.