A structured dietary approach combines plant-based eating with the specific needs of individuals managing diabetes. It involves carefully selecting foods that control blood glucose levels while adhering to vegan principles, excluding all animal products. An example includes a meal consisting of lentil soup, a mixed green salad with a vinaigrette dressing, and a serving of quinoa.
This nutritional strategy offers potential advantages for diabetic individuals, including improved glycemic control, weight management, and reduced risk of cardiovascular disease. Its origins lie in the growing awareness of the health benefits associated with both plant-based diets and diabetes management strategies, evolving as research highlights their synergistic effects.
The subsequent sections will delve into the specific components of such a dietary regimen, provide guidelines for meal planning, and address potential nutritional considerations. Strategies for long-term adherence and practical tips for successful implementation will also be discussed.
Essential Guidance
Effective management of diabetes through plant-based nutrition requires careful planning and attention to detail. The following tips provide guidance for individuals seeking to adopt this approach.
Tip 1: Prioritize Whole, Unprocessed Foods: Focus on incorporating whole grains, legumes, vegetables, and fruits into the daily diet. These foods are generally lower in glycemic index and provide essential nutrients.
Tip 2: Monitor Carbohydrate Intake: While not eliminating carbohydrates, careful monitoring of intake is essential. Choose complex carbohydrates over simple sugars and distribute carbohydrate consumption evenly throughout the day.
Tip 3: Emphasize Fiber-Rich Foods: High-fiber foods, such as beans, lentils, and oats, promote satiety, slow glucose absorption, and contribute to improved blood sugar control.
Tip 4: Incorporate Healthy Fats: Include sources of unsaturated fats, such as avocados, nuts, seeds, and olive oil, to support overall health and well-being. Limit saturated and trans fats.
Tip 5: Pay Attention to Portion Sizes: Controlling portion sizes is crucial for managing caloric intake and preventing excessive blood glucose spikes. Use measuring cups and food scales as needed.
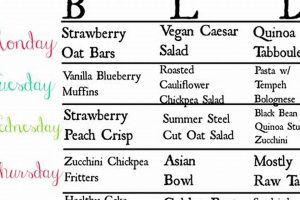
Tip 6: Plan Meals in Advance: Meal planning helps ensure adherence to the dietary guidelines and reduces the likelihood of impulsive food choices that may negatively impact blood sugar levels.
Tip 7: Consult with a Registered Dietitian: A registered dietitian with expertise in both diabetes and plant-based nutrition can provide personalized guidance and address any individual needs or concerns.
These strategies emphasize the importance of thoughtful food choices and consistent dietary habits for successful blood glucose management.
The concluding section will synthesize the key points discussed and offer further resources for individuals interested in learning more.
1. Glycemic Control
Glycemic control represents a central objective within a plant-based dietary approach for managing diabetes. It entails maintaining stable blood glucose levels within a target range to minimize the risk of both short-term and long-term complications associated with diabetes.
- Fiber’s Role in Glucose Regulation
Dietary fiber, abundant in plant-based foods, significantly influences glycemic control. Soluble fiber slows gastric emptying and glucose absorption, mitigating postprandial glucose spikes. For instance, including a serving of lentils or oats in a meal moderates the rise in blood glucose levels compared to refined carbohydrates. This impacts long-term HbA1c levels, a key indicator of average blood glucose control.
- Impact of Carbohydrate Selection
The type of carbohydrate consumed exerts a direct effect on glycemic response. Complex carbohydrates found in whole grains, legumes, and non-starchy vegetables are digested and absorbed more slowly than simple sugars found in processed foods and sugary drinks. Choosing brown rice over white rice, for example, results in a more gradual and sustained release of glucose into the bloodstream, promoting stable blood sugar levels.
- Glycemic Index and Glycemic Load Considerations
Glycemic Index (GI) and Glycemic Load (GL) are valuable tools for assessing the impact of foods on blood glucose. GI ranks foods based on how quickly they raise blood glucose levels, while GL considers both the GI and the amount of carbohydrate per serving. Selecting foods with lower GI and GL values, such as most non-starchy vegetables and legumes, aids in maintaining steady blood sugar levels. However, it is important to remember that individual responses may vary.
- Effect of Macronutrient Balance
The proportion of carbohydrates, proteins, and fats in a meal affects glycemic control. Combining carbohydrates with protein and healthy fats slows glucose absorption and prevents rapid blood sugar spikes. For example, pairing a serving of whole-grain bread with avocado and nuts provides a more balanced macronutrient profile compared to consuming the bread alone, leading to improved glycemic control.
These facets collectively demonstrate the significant role of plant-based eating in achieving glycemic control for individuals with diabetes. By prioritizing fiber-rich foods, selecting appropriate carbohydrate sources, and considering both GI and GL values, optimal blood glucose regulation can be attained. Furthermore, the proper balance of macronutrients enhances these effects, emphasizing the importance of a holistic approach to nutritional management within such a dietary regimen.
2. Nutrient Adequacy
Nutrient adequacy is paramount when implementing a plant-based dietary approach for diabetes management. This entails ensuring sufficient intake of all essential nutrients while adhering to vegan principles and managing blood glucose levels effectively. Careful meal planning is therefore indispensable.
- Vitamin B12 Sourcing
Vitamin B12 is not naturally found in plant-based foods; therefore, supplementation or consumption of fortified foods is crucial. Insufficient B12 can lead to neurological complications and anemia, particularly concerning for individuals with diabetes already at risk for nerve damage. Regularly consuming fortified nutritional yeast or a B12 supplement is essential to mitigate this deficiency.
- Iron Absorption Strategies
While plant-based diets can be rich in iron, the non-heme iron found in plant foods is less readily absorbed than heme iron from animal sources. To enhance iron absorption, pairing iron-rich foods (e.g., spinach, lentils) with vitamin C-rich foods (e.g., citrus fruits, bell peppers) is recommended. Avoiding consumption of tea or coffee with meals, as tannins can inhibit iron absorption, is also advisable.
- Omega-3 Fatty Acid Intake
Plant-based sources of omega-3 fatty acids primarily include alpha-linolenic acid (ALA), found in flaxseeds, chia seeds, and walnuts. While the body can convert ALA to EPA and DHA, the conversion rate is often limited. Therefore, incorporating these sources regularly and considering an algae-based EPA/DHA supplement is prudent to support cardiovascular and neurological health, particularly important for those with diabetes who face increased cardiovascular risk.
- Calcium and Vitamin D Considerations
Calcium intake can be met through plant-based sources such as fortified plant milks, tofu, and leafy green vegetables. Vitamin D, essential for calcium absorption, is primarily obtained through sunlight exposure. However, supplementation may be necessary, particularly in regions with limited sunlight or for individuals with darker skin pigmentation, to maintain adequate vitamin D levels and support bone health.
Addressing these specific nutrient considerations within a structured dietary approach ensures its safety and efficacy for individuals managing diabetes. The integration of fortified foods, strategic food pairings, and targeted supplementation optimizes nutrient intake, promoting overall health and minimizing the risk of deficiencies that could exacerbate diabetes-related complications.
3. Portion Management
Portion management is a critical component of a plant-based dietary approach for individuals with diabetes. Precise control over food quantities consumed is essential for maintaining stable blood glucose levels and achieving optimal metabolic outcomes. This aspect directly influences glycemic control and overall health within this dietary framework.
- Impact on Glycemic Response
Exceeding recommended portion sizes, even with healthy, plant-based foods, can lead to elevated postprandial blood glucose levels. Consuming a large serving of lentils or quinoa, despite their nutritional benefits, can overwhelm the body’s ability to process the carbohydrates effectively. Strict adherence to portion guidelines is necessary to prevent hyperglycemia and promote consistent glycemic control.
- Caloric Intake and Weight Management
While plant-based diets are often associated with weight management, uncontrolled portion sizes can negate these benefits. Overconsumption of even low-calorie, plant-based foods contributes to excess caloric intake, potentially leading to weight gain and insulin resistance. Appropriate portion sizes are vital for achieving and maintaining a healthy body weight, a key factor in diabetes management.
- Balancing Macronutrient Ratios
Portion control plays a crucial role in maintaining appropriate macronutrient ratios within a plant-based dietary approach. Accurately measuring and adjusting portion sizes of carbohydrates, proteins, and fats ensures a balanced intake that supports stable blood glucose levels and overall metabolic health. This balance is especially pertinent for optimizing insulin sensitivity and preventing nutrient imbalances.
- Practical Implementation Strategies
Effective portion management requires the use of measuring tools, such as measuring cups and food scales, to accurately assess serving sizes. Pre-planning meals and snacks with pre-portioned containers can help individuals adhere to recommended portion sizes. Mindful eating practices, focusing on satiety cues, also aid in preventing overconsumption. These strategies are crucial for consistent and sustainable adherence to a dietary regimen promoting glycemic control.
The principles of portion management, when diligently applied within a plant-based framework, serve as a cornerstone for effective diabetes management. By carefully controlling portion sizes, individuals can mitigate glycemic fluctuations, manage weight, and optimize macronutrient intake. These combined effects contribute to improved metabolic health and a reduced risk of diabetes-related complications.
4. Meal Timing
Strategic meal timing is a significant factor within a plant-based nutritional approach for managing diabetes, influencing glycemic control and metabolic regulation. Consistent intervals between meals and thoughtful distribution of carbohydrate intake can positively impact blood glucose stability.
- Frequency of Meals and Snacks
Frequent, smaller meals and snacks, rather than infrequent, larger meals, can mitigate postprandial glucose spikes. This approach prevents excessive carbohydrate intake at any one time, allowing for more gradual glucose absorption. A sample schedule could include breakfast, a mid-morning snack, lunch, an afternoon snack, and dinner, all adhering to pre-determined carbohydrate targets.
- Carbohydrate Distribution Throughout the Day
Evenly distributing carbohydrate intake throughout the day is crucial for preventing both hyperglycemia and hypoglycemia. A registered dietitian can assist in determining the appropriate carbohydrate allowance for each meal and snack, considering individual activity levels and insulin regimens. This avoids large swings in blood glucose, promoting more stable control.
- Timing of Meals Relative to Insulin Administration
For individuals using insulin, coordinating meal timing with insulin injections is essential. Rapid-acting insulin should be administered shortly before or after a meal, depending on the specific insulin type and individual response. This synchronization ensures that insulin is available to counteract the glucose surge from the meal, preventing postprandial hyperglycemia.
- Impact of Late-Night Eating
Late-night eating, particularly of carbohydrate-rich foods, can negatively impact blood glucose control. The body’s insulin sensitivity tends to decrease later in the day, making it more difficult to process glucose effectively. Avoiding large meals or snacks close to bedtime can improve overnight glucose stability and promote better overall glycemic control.
Adherence to structured meal timing, combined with careful carbohydrate distribution and coordination with insulin therapy when applicable, supports enhanced glycemic control in individuals following a plant-based diet for diabetes management. These strategies, when implemented consistently, contribute to long-term metabolic health and a reduced risk of diabetes-related complications.
5. Recipe Variety
The integration of diverse recipes is paramount to the long-term success and sustainability of a plant-based dietary strategy for managing diabetes. A lack of variety can lead to dietary monotony, potentially resulting in decreased adherence and compromised nutrient intake. Recipe diversity provides both nutritional completeness and enhanced palatability, crucial for maintaining engagement with the meal plan.
- Ensuring Nutritional Completeness
Different plant-based foods offer distinct nutrient profiles. A varied repertoire of recipes increases the likelihood of consuming a wide spectrum of vitamins, minerals, and phytonutrients essential for overall health and diabetes management. For example, rotating through recipes featuring different legumes (lentils, chickpeas, black beans) ensures a range of fiber, protein, and micronutrients that a single legume might not provide in sufficient quantities. This rotational approach mitigates the risk of nutrient deficiencies.
- Enhancing Palatability and Adherence
Dietary monotony is a significant barrier to long-term adherence to any dietary plan, including plant-based approaches for diabetes. A wide variety of recipes can stimulate appetite, prevent boredom, and make the dietary plan more enjoyable. Exploring different cuisines and cooking methods allows individuals to discover a range of flavors and textures that can sustain their interest in plant-based eating. Regular incorporation of new and appealing recipes increases the likelihood of sticking to the diet long-term.
- Optimizing Glycemic Control Through Food Combinations
Different recipes allow for strategic food combinations that can optimize glycemic control. Combining high-fiber foods with sources of healthy fats and protein slows glucose absorption and prevents rapid blood sugar spikes. For example, a recipe featuring whole grains, non-starchy vegetables, and nuts or seeds offers a balanced macronutrient profile that supports stable blood glucose levels. Diversifying recipes enables experimentation with various combinations to identify those that best suit individual metabolic needs.
- Facilitating Adaptation to Individual Preferences and Cultural Backgrounds
A versatile recipe collection allows for adaptation to individual taste preferences and cultural dietary traditions. This customization is essential for making the dietary plan feel personally relevant and sustainable. Incorporating familiar flavors and culinary techniques from one’s cultural background can enhance enjoyment and promote long-term adherence. Modification of existing recipes to align with vegan and diabetic-friendly principles allows for a more seamless integration of the dietary plan into daily life.
In summary, recipe variety is not merely an aesthetic consideration but an essential component of a successful plant-based diet for managing diabetes. It ensures nutritional completeness, enhances palatability, optimizes glycemic control through strategic food combinations, and facilitates adaptation to individual preferences and cultural backgrounds. The consistent incorporation of diverse, well-planned recipes is critical for promoting long-term adherence and improving health outcomes.
6. Blood Monitoring
Blood glucose monitoring is an indispensable component of a nutritional approach for managing diabetes. The rigorous self-monitoring of blood glucose provides real-time feedback on the effectiveness of dietary modifications and informs adjustments to the regimen. This proactive approach allows for personalized management, optimizing glycemic control and mitigating the risk of complications. Data from blood glucose measurements directly reflects the impact of food choices on blood sugar levels.
For individuals following a dietary approach, blood monitoring enables the identification of specific foods or meal combinations that may cause undesirable glucose fluctuations. For example, an individual may discover that a particular quantity of a certain fruit leads to an excessive postprandial glucose spike, prompting a reduction in portion size or a change in meal composition. Similarly, monitoring can reveal the beneficial effects of incorporating specific high-fiber foods or engaging in physical activity after meals. Consistent data collection facilitates informed decision-making regarding food selection, meal timing, and medication adjustments, with proper healthcare professional guidance.
In conclusion, blood glucose monitoring serves as the cornerstone for effective dietary management of diabetes. It provides actionable insights, allows for personalized adjustments, and promotes informed decision-making, all contributing to improved glycemic control and enhanced overall health. Regular and diligent blood monitoring, coupled with expert guidance, is essential for maximizing the benefits and minimizing the risks associated with a nutritional approach for diabetes.
7. Professional Guidance
The implementation of a vegan dietary approach for individuals managing diabetes necessitates professional oversight to ensure safety, nutritional adequacy, and optimal glycemic control. The complexities of both vegan nutrition and diabetes management warrant the expertise of qualified healthcare professionals to mitigate potential risks and maximize health benefits.
- Personalized Meal Planning
Registered dietitians specializing in diabetes and plant-based nutrition can create individualized meal plans tailored to meet specific nutritional needs, glycemic targets, and lifestyle factors. These plans account for individual preferences, cultural backgrounds, and medical conditions, promoting adherence and optimizing outcomes. The guidance ensures the diet effectively manages blood sugar levels.
- Nutrient Deficiency Prevention
Healthcare professionals can assess and address potential nutrient deficiencies that may arise from a vegan diet, such as vitamin B12, iron, calcium, and omega-3 fatty acids. Appropriate supplementation strategies and dietary modifications are recommended to prevent deficiencies and maintain optimal health. Early identification and intervention are critical.
- Medication Management and Coordination
Physicians and diabetes educators can coordinate medication adjustments with dietary changes to optimize glycemic control. Close monitoring of blood glucose levels and medication dosages is essential to prevent hypoglycemia or hyperglycemia. The professional collaboration ensures the dietary changes safely integrate with pharmaceutical interventions.
- Education and Long-Term Support
Certified diabetes educators provide comprehensive education on diabetes self-management skills, including blood glucose monitoring, carbohydrate counting, and healthy eating strategies. Ongoing support and counseling help individuals maintain long-term adherence to the dietary plan and address any challenges that may arise. Continuous education empowers individuals.
In summary, professional guidance is indispensable for the safe and effective implementation of a vegan dietary approach for individuals with diabetes. Personalized meal planning, nutrient deficiency prevention, medication management, and ongoing education are all essential components of comprehensive professional support, contributing to improved health outcomes and long-term well-being. Engagement with qualified healthcare providers ensures a tailored and sustainable dietary strategy.
Frequently Asked Questions
This section addresses common inquiries regarding the adoption of a plant-based eating strategy for managing diabetes. The information provided seeks to clarify prevalent concerns and offer evidence-based insights.
Question 1: Is a vegan diet suitable for individuals with diabetes?
A well-planned plant-based dietary approach can be appropriate for individuals with diabetes. However, diligent planning and professional guidance are essential to ensure nutritional adequacy and optimize glycemic control. This requires careful attention to macro- and micronutrient intake and consistent monitoring of blood glucose levels.
Question 2: What are the primary benefits of a vegan diabetic meal plan?
Potential benefits include improved glycemic control, weight management, reduced risk of cardiovascular disease, and enhanced insulin sensitivity. These advantages stem from the high fiber content, low saturated fat content, and abundance of beneficial phytonutrients found in plant-based foods. Individual results may vary.
Question 3: What are the potential risks associated with a vegan diet for diabetics?
Potential risks include nutrient deficiencies, such as vitamin B12, iron, calcium, and omega-3 fatty acids. Insufficient protein intake and inadequate blood glucose management are additional concerns. Careful planning, supplementation, and regular monitoring are crucial to mitigate these risks.
Question 4: How can I ensure adequate protein intake on a vegan diabetic meal plan?
Plant-based protein sources include legumes, tofu, tempeh, nuts, seeds, and whole grains. Incorporating a variety of these foods into daily meals helps meet protein requirements. Consulting a registered dietitian for personalized recommendations is advisable.
Question 5: Are all plant-based foods suitable for diabetics?
Not all plant-based foods are equally suitable. Processed vegan foods, sugary beverages, and refined carbohydrates can negatively impact blood glucose levels. Prioritizing whole, unprocessed plant foods, such as vegetables, fruits, legumes, and whole grains, is essential for maintaining glycemic control.
Question 6: How frequently should blood glucose levels be monitored on a vegan diabetic meal plan?
The frequency of blood glucose monitoring depends on individual factors, including medication regimen, glycemic control, and overall health status. Regular monitoring, as directed by a healthcare professional, is crucial for making informed dietary adjustments and preventing complications.
These answers emphasize the need for careful consideration and expert consultation when adopting a plant-based strategy for managing diabetes. The potential benefits are significant, but vigilant attention to detail is critical for achieving optimal outcomes.
The subsequent section will provide practical strategies for successfully implementing and maintaining such a dietary plan.
Conclusion
This exploration has underscored the complexities and potential benefits inherent in the implementation of a vegan diabetic meal plan. Careful planning, nutritional awareness, and consistent monitoring emerge as critical components for success. The strategic combination of whole foods, portion control, and professional guidance are essential for achieving optimal glycemic control and mitigating potential risks.
The decision to adopt such a dietary approach warrants serious consideration and a commitment to ongoing education. Further research and individual consultations with qualified healthcare professionals remain paramount in navigating the intricacies of this specialized dietary strategy. The pursuit of improved health outcomes necessitates a balanced and informed approach.