A nutritional strategy focused on plant-based eating, tailored for individuals managing diabetes, necessitates careful consideration of macronutrient ratios and glycemic impact. It involves eliminating all animal products while prioritizing whole grains, legumes, vegetables, and fruits with lower sugar content to maintain stable blood glucose levels. Example meals might include lentil soup with whole-grain bread, tofu stir-fry with brown rice, or a chickpea salad sandwich on whole wheat.
Adopting such a regimen can offer multiple advantages. Studies indicate potential improvements in insulin sensitivity, blood lipid profiles, and weight management, which are all critical aspects of diabetes control. Historically, plant-based diets have been associated with reduced risk of chronic diseases, and this specific adaptation aims to harness those benefits while addressing the unique dietary requirements of diabetic individuals. It focuses on optimizing nutrient intake and blood sugar regulation.
Subsequent sections will elaborate on the specific food groups to prioritize, meal planning techniques, and potential challenges in adopting this eating pattern. Further discussion will address the importance of consulting with registered dietitians or healthcare providers to ensure adequate nutrient intake and appropriate medication adjustments for optimal management of blood glucose levels. A comprehensive overview of long-term considerations and potential dietary modifications will also be presented.
Guiding Principles for Vegan Diabetics
The following recommendations serve as a guide for individuals pursuing a plant-based nutritional approach while managing diabetes. Adherence to these principles requires consistent monitoring and professional guidance.
Tip 1: Prioritize Low Glycemic Index Foods: Select carbohydrates that release glucose slowly into the bloodstream. Examples include legumes (lentils, beans), non-starchy vegetables (broccoli, spinach), and whole grains (quinoa, brown rice). Avoid refined grains and sugary beverages.
Tip 2: Emphasize Fiber Intake: Soluble and insoluble fiber contribute to blood sugar control and satiety. Include generous portions of vegetables, fruits, and legumes in each meal. Flax seeds and chia seeds are excellent sources of soluble fiber.
Tip 3: Incorporate Healthy Fats: While limiting saturated fats, ensure sufficient intake of unsaturated fats from sources like avocados, nuts, seeds, and olive oil. These fats support overall health and can improve insulin sensitivity.
Tip 4: Monitor Protein Consumption: Adequate protein intake is crucial for maintaining muscle mass and stabilizing blood sugar. Plant-based protein sources include tofu, tempeh, edamame, lentils, and beans. Consider protein supplementation if necessary, under professional guidance.
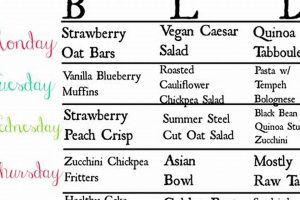
Tip 5: Plan Meals Strategically: Structure meals to include a balance of carbohydrates, protein, and fat. This helps prevent blood sugar spikes and crashes. Utilize portion control to manage overall calorie intake.
Tip 6: Regularly Monitor Blood Glucose: Frequent blood glucose monitoring is essential for adjusting dietary intake and medication dosages. Maintain a log of blood glucose readings and share this information with a healthcare provider.
Tip 7: Seek Professional Guidance: Consult with a registered dietitian specializing in diabetes and vegan nutrition. A personalized meal plan can address individual needs and minimize potential nutrient deficiencies.
Adhering to these principles, alongside consistent medical supervision, can facilitate effective diabetes management while embracing a plant-based lifestyle. Careful planning and vigilant monitoring are paramount for achieving optimal outcomes.
The subsequent discussion will explore strategies for addressing potential challenges and ensuring long-term sustainability of a plant-based dietary approach for diabetic individuals.
1. Macronutrient Balance
Macronutrient balance is a critical determinant of success for a plant-based nutritional approach aimed at managing diabetes. The precise ratio of carbohydrates, proteins, and fats directly influences postprandial glucose levels and overall metabolic stability. An improperly balanced plant-based dietary strategy may lead to either hyperglycemia or hypoglycemia, negating the potential benefits of the dietary pattern. For example, a meal consisting primarily of high-carbohydrate, low-protein plant foods could trigger a significant glucose spike, while a diet deficient in essential fats may compromise insulin sensitivity over time. The careful manipulation of macronutrient ratios, considering the specific needs of the individual, is therefore paramount.
Practical application of macronutrient balance within this context involves prioritizing whole, unprocessed plant foods and strategically combining them to achieve target ratios. For instance, a balanced meal might consist of lentils (protein and complex carbohydrates), quinoa (complex carbohydrates), and avocado (healthy fats). Monitoring blood glucose levels after meals is essential to assess the impact of specific food combinations and adjust macronutrient proportions accordingly. Additionally, individuals must be aware of the carbohydrate content of various plant foods and make informed choices to avoid excessive intake, even from seemingly healthy sources such as fruits and starchy vegetables. Protein needs must be addressed with conscious dietary choices.
In conclusion, macronutrient balance represents a foundational element of a successful plant-based dietary approach for individuals with diabetes. Achieving this balance requires careful planning, informed food choices, and regular monitoring of blood glucose levels. While the benefits of such a dietary pattern are well-documented, the inherent challenges related to meeting macronutrient requirements from plant sources necessitate ongoing education and, ideally, guidance from a registered dietitian or healthcare professional. Long-term adherence depends on both the effective implementation of these principles and the individual’s ability to adapt the dietary pattern to their specific needs and preferences.
2. Glycemic Index Awareness
Glycemic Index (GI) awareness constitutes a cornerstone of effective dietary management for individuals with diabetes, particularly when adopting a plant-based nutritional strategy. Understanding the GI of various foods is paramount to mitigating postprandial hyperglycemia and maintaining stable blood glucose levels. The inherently carbohydrate-rich nature of many plant-based foods necessitates a conscious focus on GI values to optimize metabolic control.
- GI Values and Food Selection
The GI ranks carbohydrate-containing foods based on their effect on blood glucose levels after consumption. High-GI foods cause rapid and substantial glucose spikes, while low-GI foods result in a more gradual and sustained increase. In the context of a plant-based eating pattern for diabetes management, this understanding guides the selection of carbohydrate sources. For instance, opting for brown rice (lower GI) over white rice (higher GI) can contribute to better glucose regulation. Similarly, choosing whole fruits over fruit juices, due to the presence of fiber, will result in a lower glycemic response.
- Impact of Food Preparation
The method of food preparation can influence the GI of a food. For example, cooking pasta al dente, rather than overcooking it, reduces its GI. Likewise, processing or refining grains increases their GI. Individuals must be aware of these variations and adjust their food preparation techniques accordingly. In a plant-based framework, this may involve emphasizing minimally processed foods and employing cooking methods that preserve the integrity of the carbohydrates.
- Role of Fiber and Protein
The presence of fiber and protein in a meal can modulate the glycemic response to carbohydrates. Fiber slows down the absorption of glucose, while protein can stimulate insulin secretion and enhance glucose uptake by cells. Incorporating high-fiber plant foods, such as legumes and non-starchy vegetables, and adequate sources of plant-based protein, such as tofu and tempeh, can mitigate the impact of carbohydrate consumption on blood glucose levels. A balanced meal composition is therefore crucial.
- Practical Application in Meal Planning
Glycemic index awareness should inform all aspects of meal planning. This includes considering the GI of individual ingredients and the overall glycemic load of the meal. A dietary strategy should not only focus on selecting low-GI foods but also on combining them in a manner that optimizes glucose control. Regular monitoring of blood glucose levels after meals is essential to assess the effectiveness of meal plans and make necessary adjustments. Consulting with a registered dietitian specializing in diabetes and plant-based nutrition can provide personalized guidance in this regard.
In essence, glycemic index awareness empowers individuals pursuing a plant-based dietary strategy to make informed food choices that support effective diabetes management. This knowledge, coupled with consistent blood glucose monitoring and professional guidance, represents a vital component of a comprehensive approach to achieving optimal metabolic health. The principles discussed highlight the need to go beyond simply adopting a vegan diet and emphasizes the importance of understanding the nuances of carbohydrate metabolism within that framework.
3. Fiber Rich Foods
The inclusion of fiber-rich foods is a central tenet of a plant-based dietary strategy for managing diabetes. The physiological effects of dietary fiber directly address key challenges in glycemic control, insulin sensitivity, and satiety, making it an indispensable component of the nutritional approach.
- Glycemic Control Enhancement
Soluble fiber, abundant in legumes, oats, and certain fruits, slows gastric emptying and glucose absorption. This attenuates postprandial blood glucose spikes, a critical factor in managing diabetes. For example, incorporating a serving of lentils into a meal moderates the blood sugar response compared to consuming refined grains alone. This translates to improved HbA1c levels over time, a key indicator of long-term glycemic control.
- Insulin Sensitivity Improvement
Studies suggest that high-fiber diets can improve insulin sensitivity. The mechanisms are complex and may involve alterations in gut microbiota and reduced inflammation. Regularly consuming fiber-rich foods, such as whole grains and vegetables, supports optimal insulin function. This is especially important for individuals with type 2 diabetes, who often exhibit insulin resistance.
- Satiety and Weight Management
Fiber increases satiety, promoting reduced calorie intake and aiding in weight management. This is particularly beneficial for individuals with diabetes, as obesity can exacerbate insulin resistance and complicate blood sugar control. High-fiber plant foods, such as non-starchy vegetables, provide bulk with minimal caloric impact, fostering a sense of fullness and reducing the likelihood of overeating.
- Lipid Profile Modulation
Soluble fiber can lower LDL cholesterol levels, a significant risk factor for cardiovascular disease, a common comorbidity in individuals with diabetes. By binding to bile acids in the digestive tract, fiber promotes their excretion, prompting the liver to utilize cholesterol to produce more bile acids. This contributes to a reduction in circulating cholesterol levels. Foods like oats, beans, and psyllium are particularly effective in this regard.
The benefits derived from fiber-rich foods are integral to the efficacy of a plant-based diet in managing diabetes. Strategic inclusion of these foods supports stable blood glucose levels, improved insulin sensitivity, weight management, and cardiovascular health. Individuals adopting a plant-based nutritional strategy should prioritize a diverse range of fiber sources to maximize these advantages. While a shift towards plant-based eating can be beneficial, focusing on fiber ensures that the benefits are effectively realized in the context of diabetic management.
4. Protein Source Variety
Adequate protein intake is critical for managing diabetes, and within a plant-based framework, securing sufficient protein necessitates a diverse range of protein sources. Variety ensures the intake of complete proteins and a broad spectrum of amino acids, essential for maintaining muscle mass, supporting metabolic function, and optimizing glycemic control.
- Amino Acid Profile Completeness
Plant-based protein sources often lack one or more essential amino acids, rendering them incomplete proteins. Combining different protein sources throughout the day ensures the consumption of all essential amino acids. For example, pairing legumes (e.g., lentils, beans) with grains (e.g., quinoa, brown rice) creates a complete protein profile. In a plant-based eating pattern, a lack of variety could lead to deficiencies, hindering muscle maintenance and overall health.
- Impact on Satiety and Glucose Regulation
Protein plays a significant role in promoting satiety, which is crucial for weight management and glucose control. Different plant-based proteins may have varying effects on satiety. Incorporating a diverse array, such as tofu, tempeh, edamame, nuts, and seeds, can enhance satiety and stabilize blood glucose levels. Monotonous protein intake could result in inadequate satiety and increased fluctuations in blood sugar.
- Nutrient Diversity and Absorption
Different plant-based proteins offer unique combinations of vitamins, minerals, and phytonutrients. Consuming a variety of these sources maximizes the intake of essential micronutrients and promotes overall health. For example, nuts and seeds provide healthy fats and minerals, while legumes are rich in iron and fiber. Limited protein source variety can lead to deficiencies in specific nutrients, compromising overall well-being.
- Digestibility and Tolerance
Individuals may experience varying levels of digestibility and tolerance to different plant-based proteins. Some may find legumes difficult to digest, while others may be sensitive to soy. Offering a range of options allows for personalized adjustments based on individual needs and preferences, promoting long-term adherence to the nutritional approach. A rigid, limited protein selection may result in gastrointestinal discomfort and decreased compliance.
The integration of diverse plant-based protein sources is not merely a matter of dietary preference but a fundamental principle for optimizing a plant-based diet in the context of diabetes management. Variety ensures complete protein intake, enhances satiety, promotes nutrient diversity, and accommodates individual tolerance levels. Each facet plays a vital role in supporting effective glycemic control and overall health within a carefully constructed plan.
5. Micronutrient Sufficiency
Micronutrient sufficiency is a critical consideration within a vegan dietary strategy designed for diabetes management. The restricted nature of both the vegan and diabetic diets necessitates careful planning to ensure adequate intake of essential vitamins and minerals. Failure to address micronutrient needs can lead to deficiencies, exacerbating existing health challenges associated with diabetes and potentially undermining the benefits of the dietary approach.
- Vitamin B12 Intake
Vitamin B12 is primarily found in animal products; therefore, individuals following a vegan diet must obtain it through fortified foods or supplements. Deficiency can lead to neurological complications and macrocytic anemia, conditions that can be particularly problematic in individuals with diabetes. Monitoring B12 levels is essential, and supplementation should be considered to maintain adequate status.
- Iron Bioavailability
While plant-based diets can be rich in iron, the non-heme iron found in plants is less readily absorbed than heme iron from animal sources. Individuals with diabetes may have compromised iron absorption, making it crucial to consume iron-rich plant foods in combination with vitamin C to enhance absorption. Examples include spinach with lemon juice or lentils with tomatoes. Iron deficiency anemia can further impair glycemic control and exacerbate fatigue.
- Calcium and Vitamin D Status
Dairy products are a primary source of calcium, and while plant-based sources exist (e.g., fortified plant milks, leafy green vegetables), adequate intake may require conscious effort. Vitamin D, crucial for calcium absorption, is often obtained through sun exposure or supplementation. Deficiencies in calcium and vitamin D can increase the risk of osteoporosis and impair insulin secretion. Fortified plant milks and supplementation, when necessary, are essential for maintaining bone health and metabolic function.
- Omega-3 Fatty Acid Considerations
While a vegan diet can provide alpha-linolenic acid (ALA), a precursor to omega-3 fatty acids, the conversion of ALA to EPA and DHA (the more biologically active forms of omega-3s) can be limited. DHA is particularly important for brain health and inflammation management. Individuals may consider algal oil supplements to ensure adequate DHA intake, especially given the increased cardiovascular risk associated with diabetes.
Addressing micronutrient sufficiency in a plant-based dietary approach for diabetes requires proactive planning, informed food choices, and, in many cases, strategic supplementation. Vigilant monitoring of nutrient status, in consultation with a registered dietitian or healthcare provider, is crucial to mitigate the risk of deficiencies and optimize the overall health benefits of this dietary strategy. The interplay between carefully managing blood glucose and achieving micronutrient adequacy is essential for the effective long-term diabetic management.
6. Meal Timing & Frequency
Meal timing and frequency represent critical elements in the effective implementation of a plant-based dietary strategy for diabetes management. These factors significantly influence postprandial glucose levels, insulin sensitivity, and overall metabolic stability, necessitating careful consideration for individuals adhering to a vegan diabetic meal plan. Strategic meal timing and frequency can mitigate hyperglycemic excursions and optimize the utilization of nutrients, contributing to improved glycemic control.
- Consistent Meal Intervals
Maintaining consistent meal intervals throughout the day helps to regulate blood glucose levels and prevent extreme fluctuations. Irregular eating patterns can lead to both hyperglycemia and hypoglycemia, complicating diabetes management. For individuals following a vegan diabetic meal plan, establishing a regular schedule with meals and snacks at predictable times ensures a steady supply of nutrients and minimizes glycemic variability. For example, a consistent eating pattern might involve meals at 8 AM, 12 PM, and 6 PM, with snacks at 10 AM and 3 PM, tailored to individual needs and medication regimens.
- Carbohydrate Distribution
Even distribution of carbohydrate intake across meals and snacks is essential for optimal glycemic control. Consuming large amounts of carbohydrates in a single meal can overwhelm the body’s ability to process glucose, leading to hyperglycemia. Conversely, inadequate carbohydrate intake can result in hypoglycemia, particularly for individuals taking insulin or oral hypoglycemic agents. A vegan diabetic meal plan should emphasize the strategic distribution of carbohydrates, focusing on low glycemic index sources, to promote stable blood glucose levels throughout the day. For instance, a breakfast consisting of oatmeal with berries and nuts provides a balanced carbohydrate load compared to a high-carbohydrate option like fruit juice and white toast.
- Pre- and Post-Exercise Nutrition
Meal timing in relation to physical activity is crucial for individuals with diabetes. Consuming a small carbohydrate-containing snack before exercise can prevent hypoglycemia, while a post-exercise meal or snack replenishes glycogen stores and stabilizes blood glucose levels. A vegan diabetic meal plan should incorporate appropriate pre- and post-exercise nutrition strategies, using whole, unprocessed plant foods to optimize performance and glycemic control. Examples include a piece of fruit or a handful of nuts before exercise and a combination of carbohydrates and protein, such as a lentil soup with whole-grain bread, after exercise.
- Evening Meal Composition
The composition of the evening meal can significantly impact overnight blood glucose levels. A high-fat or high-carbohydrate meal consumed close to bedtime can lead to elevated morning glucose levels. A vegan diabetic meal plan should prioritize a balanced evening meal with adequate protein, fiber, and complex carbohydrates to promote stable overnight glucose levels. Examples include a tofu stir-fry with brown rice and vegetables or a chickpea curry with quinoa. Avoiding sugary desserts and processed foods in the evening is essential for preventing nocturnal hyperglycemia.
In conclusion, meal timing and frequency are integral components of a successful vegan diabetic meal plan. Strategically managing these factors, in conjunction with careful food selection and portion control, contributes to improved glycemic control, enhanced insulin sensitivity, and overall metabolic stability. Individuals following this dietary approach should prioritize consistent meal intervals, even carbohydrate distribution, appropriate pre- and post-exercise nutrition, and a balanced evening meal composition to optimize their health outcomes. Monitoring blood glucose levels and consulting with a registered dietitian or healthcare provider are essential for tailoring meal timing and frequency to individual needs and preferences. The synergistic effect of dietary composition and structured meal timing creates the most effective plan.
7. Professional Consultation
The adoption of a vegan diabetic meal plan necessitates the involvement of qualified healthcare professionals. While the potential benefits of such a diet are recognized, its implementation requires careful consideration of individual health status, dietary needs, and medication management. A professional consultation ensures that the diet is both nutritionally adequate and safe for individuals managing diabetes.
- Personalized Meal Planning
Registered dietitians, specifically those with expertise in both vegan nutrition and diabetes management, can develop personalized meal plans. These plans account for individual caloric needs, macronutrient ratios, and glycemic control goals. A generic meal plan may not adequately address the specific requirements of each individual, potentially leading to nutrient deficiencies or unstable blood glucose levels. A dietitian can assess current dietary habits, medical history, and lifestyle factors to create a tailored approach that maximizes benefits and minimizes risks. For example, a consultation might reveal a need for increased iron or vitamin B12 intake, prompting the dietitian to incorporate specific fortified foods or supplements into the meal plan.
- Medication Management and Adjustment
Changes in dietary intake can significantly impact blood glucose levels and, consequently, the need for medication adjustments. Healthcare providers, including physicians and certified diabetes educators, play a crucial role in monitoring blood glucose patterns and adjusting medication dosages accordingly. Adopting a vegan diabetic meal plan often requires a reduction in insulin or oral hypoglycemic agents to prevent hypoglycemia. A professional consultation ensures that these adjustments are made safely and effectively, based on individual blood glucose readings and metabolic responses. Neglecting medication adjustments can lead to dangerous fluctuations in blood sugar levels.
- Nutrient Deficiency Screening and Prevention
Vegan diets can be deficient in certain nutrients, such as vitamin B12, iron, calcium, and omega-3 fatty acids. Individuals with diabetes may be at increased risk for nutrient deficiencies due to medication side effects or impaired nutrient absorption. A healthcare professional can assess nutrient status through blood tests and recommend appropriate supplementation to prevent deficiencies. This proactive approach helps to maintain overall health and prevent complications associated with diabetes and nutrient deficiencies. For instance, a consultation might identify a need for vitamin D supplementation, especially in individuals with limited sun exposure.
- Ongoing Monitoring and Support
Diabetes management is an ongoing process that requires regular monitoring and support. Healthcare professionals can provide ongoing education, address challenges, and make adjustments to the meal plan as needed. This continuous support ensures that individuals remain adherent to the diet and achieve their glycemic control goals. Regular consultations allow for early identification and management of any issues that may arise, promoting long-term success with the vegan diabetic meal plan. This support also ensures adherence to a new diet plan.
The involvement of healthcare professionals is essential for the safe and effective implementation of a vegan diabetic meal plan. Personalized meal planning, medication management, nutrient deficiency screening, and ongoing monitoring contribute to improved glycemic control, nutrient adequacy, and overall health. This collaboration between individuals and healthcare providers maximizes the benefits of the diet while minimizing potential risks.
Frequently Asked Questions
The following addresses prevalent inquiries regarding the application and implications of a plant-based eating strategy for individuals managing diabetes. This seeks to offer clarity on common concerns and misconceptions.
Question 1: Is a plant-based diet inherently suitable for managing diabetes?
A plant-based dietary pattern, when appropriately structured, can offer significant benefits for diabetes management. Emphasis on low glycemic index carbohydrates, adequate protein intake, and strategic fat consumption is crucial. A poorly planned diet may lead to nutrient deficiencies or erratic blood sugar control.
Question 2: Are there specific nutrient concerns when following a plant-based approach with diabetes?
Particular attention must be paid to vitamin B12, iron, calcium, vitamin D, omega-3 fatty acids, and zinc. Plant-based diets inherently lack vitamin B12, necessitating supplementation or fortified food consumption. The bioavailability of iron and calcium from plant sources is lower, requiring strategic dietary choices. Monitoring nutrient status and addressing deficiencies through supplementation is essential.
Question 3: How does a plant-based meal plan affect medication requirements for diabetes?
The implementation of a plant-based dietary strategy often necessitates adjustments in medication dosages, particularly for insulin and oral hypoglycemic agents. The improved insulin sensitivity and reduced carbohydrate intake associated with this diet can lead to hypoglycemia if medication dosages are not appropriately reduced. Close collaboration with a healthcare provider is essential to monitor blood glucose levels and adjust medication regimens accordingly.
Question 4: What are the primary sources of protein in a plant-based diabetic diet?
Suitable protein sources include legumes (lentils, beans, chickpeas), tofu, tempeh, edamame, nuts, seeds, and plant-based protein powders. Combining different protein sources throughout the day ensures the intake of all essential amino acids. Adequate protein intake is crucial for maintaining muscle mass and supporting metabolic function.
Question 5: How does fiber intake impact glycemic control in this diet?
Dietary fiber, abundant in plant-based foods, slows gastric emptying and glucose absorption, attenuating postprandial blood glucose spikes. Soluble fiber can also improve insulin sensitivity and lower LDL cholesterol levels. Prioritizing high-fiber plant foods, such as legumes, whole grains, and non-starchy vegetables, is essential for effective glycemic control.
Question 6: Can a plant-based diet reverse diabetes?
While a plant-based dietary strategy can significantly improve glycemic control and reduce the need for medication, it does not guarantee the reversal of diabetes for all individuals. Remission may be possible for some individuals with early-stage type 2 diabetes, but long-term commitment to the diet and ongoing medical supervision are essential. The efficacy varies greatly based on individual factors.
These answers provide a fundamental understanding. Individualized guidance from qualified healthcare professionals is vital for the successful implementation of a plant-based approach for diabetes management.
Subsequent discussions will address practical strategies for creating sustainable vegan diabetic meal plans and addressing potential challenges in the long term.
Conclusion
The preceding exploration of a vegan diabetic diet meal plan illuminates both its potential benefits and inherent complexities. Effective implementation necessitates a deep understanding of macronutrient balance, glycemic index awareness, fiber-rich food selection, diverse protein sources, micronutrient sufficiency, and strategic meal timing. This dietary strategy demands rigorous attention to detail and should not be undertaken without proper preparation and professional guidance. The nutritional requirements are significant.
Ultimately, a properly constructed plan can offer substantial improvements in glycemic control and overall health outcomes for individuals managing diabetes. Sustained adherence to this dietary approach depends on continuous monitoring, informed decision-making, and ongoing collaboration with qualified healthcare professionals. The significance of this nutritional strategy lies in its capacity to empower individuals to actively manage their condition and potentially mitigate long-term complications. Consider this only with professional guidance.